The precision and reliability demanded in modern healthcare settings make orthopedic surgery instruments manufacturing one of the most critical sectors in medical device production. Every instrument that enters an operating room must meet exacting standards to ensure patient safety and surgical success. From titanium implants to specialized cutting tools, the manufacturing process requires adherence to international quality protocols, advanced materials science, and rigorous testing procedures that validate performance under the most demanding clinical conditions.
The global orthopedic device market continues to expand rapidly, driven by aging populations and increasing rates of sports-related injuries. This growth intensifies the focus on manufacturing excellence, as hospitals and surgical centers demand instruments that combine durability, precision, and biocompatibility. Understanding the fundamental quality standards that govern this industry provides insight into how manufacturers maintain the high standards necessary for successful patient outcomes.
Regulatory Framework and Compliance Standards
FDA Classification and Requirements
The United States Food and Drug Administration classifies orthopedic instruments into multiple categories based on risk levels and intended use. Class I devices typically include basic surgical instruments like forceps and retractors, while Class II devices encompass more complex items such as powered surgical tools and specialized implant insertion instruments. Each classification level demands specific documentation, testing protocols, and quality management systems that manufacturers must implement throughout their production processes.
Manufacturing facilities must maintain FDA registration and adhere to Good Manufacturing Practices as outlined in 21 CFR Part 820. These regulations establish comprehensive requirements for design controls, document management, corrective and preventive actions, and management responsibility. Regular FDA inspections ensure ongoing compliance, with any deviations potentially resulting in warning letters, product recalls, or manufacturing shutdowns that can severely impact business operations.
International Standards Integration
Beyond FDA requirements, successful orthopedic surgery instruments manufacturing operations must comply with international standards including ISO 13485 for medical device quality management systems. This standard provides a framework for consistent quality throughout the product lifecycle, from initial design through post-market surveillance. European markets require CE marking compliance, which involves conformity assessment procedures that demonstrate adherence to Medical Device Regulation requirements.
Japanese PMDA regulations, Health Canada requirements, and other regional standards create a complex regulatory landscape that manufacturers must navigate successfully. Companies pursuing global market access often implement harmonized quality systems that exceed individual regulatory requirements, ensuring consistent product quality regardless of destination market. This approach reduces regulatory risk while streamlining production processes across multiple manufacturing locations.
Materials Science and Biocompatibility
Advanced Alloy Selection
Material selection represents a critical decision point in orthopedic surgery instruments manufacturing, as each material must demonstrate specific mechanical properties and biocompatibility characteristics. Stainless steel grades like 316L and 420 provide excellent corrosion resistance and mechanical strength for cutting instruments, while titanium alloys offer superior biocompatibility for implantable devices. Cobalt-chromium alloys deliver exceptional wear resistance for joint replacement components that must function for decades within the human body.
Advanced ceramics and composite materials continue expanding their role in orthopedic applications, particularly for components requiring extreme hardness or specific tribological properties. Zirconia ceramic heads for hip replacements demonstrate superior wear characteristics compared to traditional materials, while carbon fiber composites provide radiolucent properties essential for imaging compatibility. Material traceability systems ensure complete documentation from raw material receipt through final product delivery, enabling rapid response to any quality issues that may arise.
Surface Treatment Technologies
Surface engineering plays a crucial role in optimizing orthopedic instrument performance through treatments that enhance biocompatibility, reduce friction, and improve corrosion resistance. Plasma spray coatings create porous surfaces that promote bone ingrowth for implant fixation, while ion beam assisted deposition produces ultra-smooth surfaces that minimize wear in articulating joints. Passivation treatments remove surface contaminants and create protective oxide layers that prevent corrosion in challenging biological environments.
Emerging surface technologies include diamond-like carbon coatings that provide exceptional hardness and biocompatibility, and antimicrobial silver coatings that reduce infection risk in implantable devices. Each surface treatment requires specific validation testing to demonstrate compatibility with intended applications, including cytotoxicity testing, corrosion testing, and mechanical property evaluation. Process validation ensures consistent surface treatment quality across production batches while maintaining traceability throughout the manufacturing sequence.
Precision Manufacturing Processes
Computer Numerical Control Machining
Modern orthopedic surgery instruments manufacturing relies heavily on advanced CNC machining centers that deliver the precision required for complex geometries and tight tolerances. Five-axis machining capabilities enable production of intricate instrument designs in single setups, reducing handling errors while improving dimensional accuracy. Tool path optimization software minimizes cycle times while maintaining surface finish requirements that are critical for proper instrument function and cleaning efficiency.
Statistical process control systems monitor machining parameters in real-time, automatically adjusting cutting conditions to maintain dimensional tolerances within specified limits. Tool wear monitoring prevents quality issues by triggering tool changes before wear patterns affect part dimensions or surface finish. Automated measurement systems provide immediate feedback on critical dimensions, enabling rapid detection and correction of any process variations that could compromise product quality.
Additive Manufacturing Integration
Three-dimensional printing technologies are revolutionizing orthopedic surgery instruments manufacturing by enabling production of patient-specific implants and complex geometries that cannot be achieved through traditional manufacturing methods. Selective laser melting and electron beam melting processes create titanium implants with controlled porosity structures that promote bone ingrowth while reducing stress shielding effects. Direct metal laser sintering produces surgical guides and custom instruments tailored to individual patient anatomy.
Quality control for additive manufacturing requires specialized approaches including powder characterization, build parameter validation, and post-processing verification. Computed tomography scanning enables non-destructive evaluation of internal structures, while mechanical testing validates that additively manufactured components meet strength and fatigue requirements. Process qualification protocols ensure consistent quality across different build orientations and geometries while maintaining traceability for each manufactured component.
Quality Assurance and Testing Protocols
Dimensional Verification Systems
Comprehensive dimensional inspection represents a cornerstone of quality assurance in orthopedic surgery instruments manufacturing, utilizing coordinate measuring machines, optical measurement systems, and specialized gauges to verify critical dimensions. Vision systems provide rapid inspection of complex geometries while maintaining measurement accuracy sufficient for medical device applications. Automated inspection cells integrate multiple measurement technologies to provide complete dimensional characterization without human intervention.
Measurement uncertainty analysis ensures that inspection systems provide adequate discrimination for specified tolerances, while gauge repeatability and reproducibility studies validate measurement system capability. Statistical analysis of measurement data identifies process trends and potential issues before they result in nonconforming products. Digital documentation systems maintain complete measurement records that support regulatory requirements and enable rapid investigation of any quality concerns.
Mechanical Property Validation
Mechanical testing protocols verify that orthopedic instruments meet strength, fatigue, and durability requirements specified in relevant standards and design specifications. Tensile testing, compression testing, and fatigue testing evaluate material properties and component performance under simulated service conditions. Specialized tests such as torque testing for bone screws and pullout testing for implant fixation elements provide specific validation for orthopedic applications.
Accelerated aging studies predict long-term performance by subjecting devices to elevated temperature and humidity conditions that simulate years of service in compressed timeframes. Biocompatibility testing including cytotoxicity, sensitization, and irritation studies ensures that materials and devices are safe for patient contact. Test method validation ensures that all testing procedures provide accurate and reproducible results that support regulatory submissions and clinical use decisions.
Sterilization and Packaging Considerations
Sterilization Method Selection
Sterilization represents a critical final step in orthopedic surgery instruments manufacturing, with method selection depending on material compatibility, device geometry, and packaging requirements. Steam sterilization using saturated steam under pressure provides effective microbial kill while maintaining material properties for most metallic instruments. Ethylene oxide sterilization accommodates temperature-sensitive materials and complex geometries that cannot be effectively sterilized using steam methods.
Gamma radiation sterilization offers advantages for single-use devices and polymer components that cannot withstand high temperatures, while electron beam sterilization provides rapid processing with minimal heat generation. Each sterilization method requires specific validation studies that demonstrate effective microbial kill while maintaining device functionality and material properties. Process monitoring and routine testing ensure continued sterilization effectiveness throughout production operations.
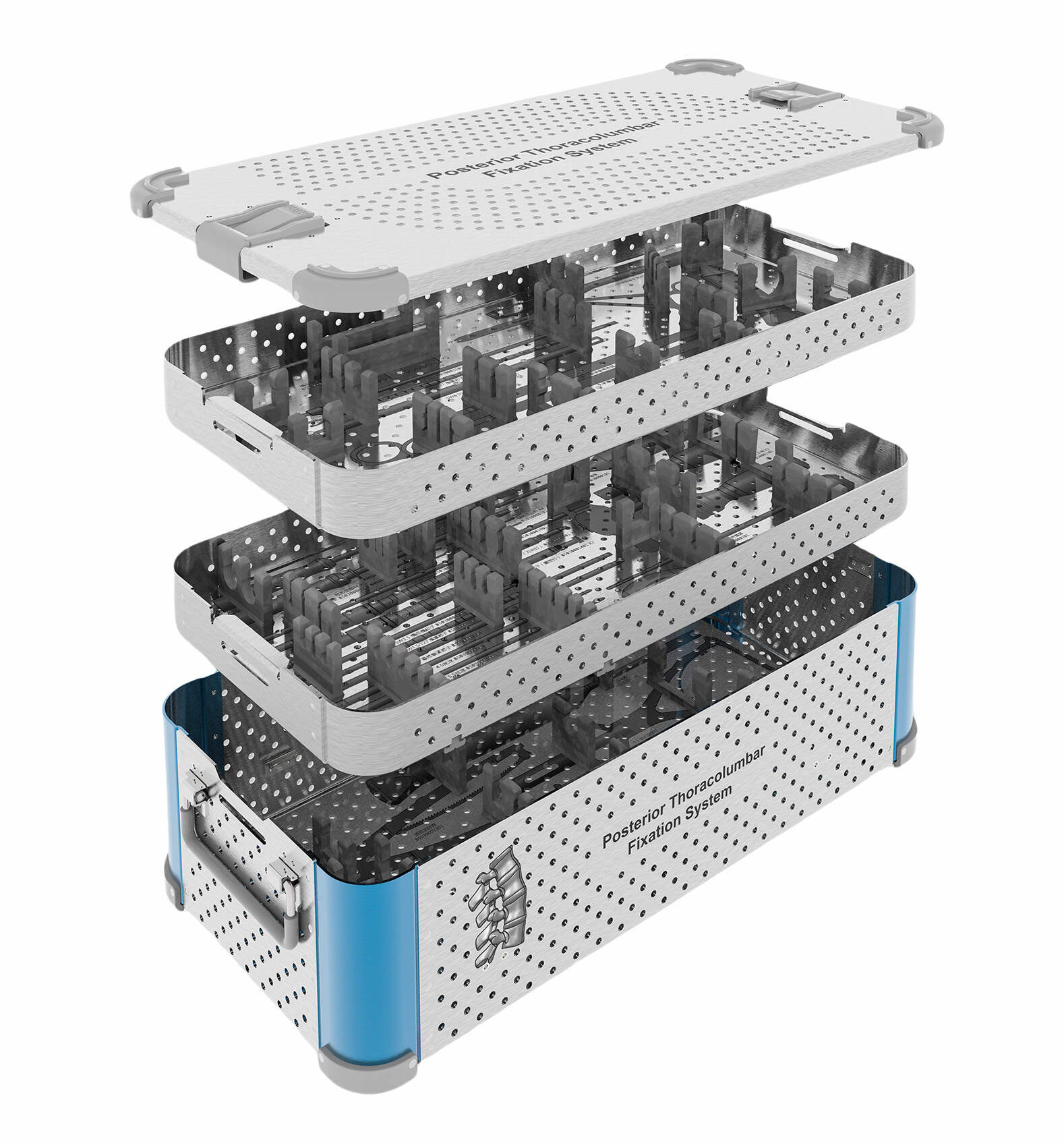
Protective Packaging Systems
Packaging design for orthopedic instruments must maintain sterility while protecting devices from damage during shipping and storage. Tyvek pouches, rigid containers, and thermoformed trays each offer specific advantages depending on device configuration and sterilization method. Barrier properties must prevent microbial contamination while allowing sterilant penetration and removal during processing cycles.
Package validation studies demonstrate seal integrity, sterile barrier maintenance, and protection from physical damage under specified storage and shipping conditions. Accelerated aging studies predict package performance over stated shelf life periods, while distribution testing validates package integrity under actual shipping conditions. Labeling requirements ensure proper device identification and provide essential information for safe device use in clinical settings.
Supply Chain Management and Traceability
Vendor Qualification Programs
Robust supplier management programs ensure that all components and materials used in orthopedic surgery instruments manufacturing meet specified quality requirements. Vendor audits evaluate quality systems, manufacturing capabilities, and regulatory compliance to identify qualified suppliers capable of supporting medical device production. Incoming inspection protocols verify that purchased materials conform to specifications before entering production processes.
Supplier performance monitoring tracks delivery performance, quality metrics, and corrective action effectiveness to maintain approved vendor status. Risk assessment procedures identify potential supply chain vulnerabilities and establish contingency plans to ensure continued production capability. Long-term supplier partnerships enable collaborative improvement initiatives that enhance quality while reducing costs through process optimization and waste reduction.
Product Traceability Systems
Complete product traceability from raw materials through final delivery enables rapid response to quality issues and supports regulatory requirements for medical device manufacturing. Unique device identifiers provide permanent marking that links each device to manufacturing records, sterilization data, and distribution information. Electronic batch records maintain detailed documentation of all manufacturing operations while enabling rapid data retrieval for investigation purposes.
Serialization systems create unique identifiers for individual devices, supporting track-and-trace capabilities throughout the supply chain. Integration with enterprise resource planning systems provides real-time visibility into inventory levels, production status, and quality metrics. Automated data capture reduces manual documentation errors while ensuring complete record accuracy that supports regulatory compliance and continuous improvement initiatives.
Continuous Improvement and Innovation
Lean Manufacturing Implementation
Lean manufacturing principles enhance efficiency in orthopedic surgery instruments manufacturing while maintaining strict quality standards required for medical devices. Value stream mapping identifies opportunities to eliminate non-value-added activities while preserving essential quality control steps. Cellular manufacturing configurations reduce work-in-process inventory and cycle times while improving quality through reduced handling and simplified material flow.
Single-minute exchange of die techniques minimize changeover times between different product configurations, enabling smaller batch sizes and improved responsiveness to customer demand variations. Visual management systems provide immediate feedback on production status and quality metrics, while standardized work procedures ensure consistent execution of critical manufacturing operations. Employee involvement programs harness workforce expertise to identify improvement opportunities and implement sustainable solutions.
Technology Integration Strategies
Digital transformation initiatives integrate advanced technologies including artificial intelligence, machine learning, and Internet of Things sensors to optimize manufacturing operations. Predictive analytics identify potential equipment failures before they occur, reducing unplanned downtime while maintaining production schedules. Real-time monitoring systems track critical process parameters and automatically adjust settings to maintain optimal operating conditions.
Digital twin technology creates virtual representations of manufacturing processes that enable simulation and optimization without disrupting production operations. Augmented reality systems provide technicians with real-time guidance for complex assembly operations while maintaining detailed documentation of all activities. Integration platforms connect disparate systems to provide unified visibility into operations while supporting data-driven decision making throughout the organization.
FAQ
What are the most critical quality standards for orthopedic instrument manufacturing
The most critical standards include FDA Good Manufacturing Practices under 21 CFR Part 820, ISO 13485 for medical device quality management systems, and specific product standards such as ASTM F899 for surgical instruments. These standards establish requirements for design controls, risk management, sterilization validation, biocompatibility testing, and comprehensive documentation throughout the manufacturing process. Compliance with these standards ensures that orthopedic instruments meet safety and effectiveness requirements for clinical use.
How do manufacturers ensure material traceability in orthopedic device production
Material traceability systems track raw materials from receipt through final product delivery using unique identifiers and electronic batch records. Certificate of analysis documentation accompanies each material lot, providing chemical composition, mechanical properties, and test results. Manufacturing execution systems link material lots to specific products, enabling rapid identification of affected devices if quality issues arise. Serialization at the device level provides additional traceability capability for individual product tracking throughout the supply chain.
What role does additive manufacturing play in modern orthopedic instrument production
Additive manufacturing enables production of patient-specific implants, complex geometries, and rapid prototyping for new device development. Technologies such as selective laser melting and electron beam melting create titanium implants with controlled porosity for enhanced bone integration. Direct metal laser sintering produces surgical guides and custom instruments tailored to individual patient anatomy. Quality control for additive manufacturing requires specialized protocols including powder characterization, process parameter validation, and non-destructive testing of finished components.
How do sterilization requirements impact orthopedic instrument design and manufacturing
Sterilization requirements significantly influence material selection, device geometry, and packaging design throughout the development process. Materials must withstand repeated sterilization cycles without degradation of mechanical properties or biocompatibility. Device designs must accommodate sterilant penetration to all surfaces while avoiding crevices that could harbor contaminants. Packaging systems must maintain sterile barriers while allowing sterilization and providing protection during storage and distribution. Validation studies demonstrate sterilization effectiveness and material compatibility for each product configuration.
Table of Contents
- Regulatory Framework and Compliance Standards
- Materials Science and Biocompatibility
- Precision Manufacturing Processes
- Quality Assurance and Testing Protocols
- Sterilization and Packaging Considerations
- Supply Chain Management and Traceability
- Continuous Improvement and Innovation
-
FAQ
- What are the most critical quality standards for orthopedic instrument manufacturing
- How do manufacturers ensure material traceability in orthopedic device production
- What role does additive manufacturing play in modern orthopedic instrument production
- How do sterilization requirements impact orthopedic instrument design and manufacturing
